What Are Descriptive and Inferential Statistics?
In medical research, data alone is not enough. Descriptive statistics organize and summarize collected data for example, showing the average blood pressure in a group of patients. Inferential statistics allow researchers to draw conclusions about a larger population based on that sample.
Both are essential for turning data into actionable insights that support clinical decisions, public health policies, and evidence-based medicine.
In medical studies, both descriptive and inferential statistics belong to the broader branch of statistics known as statistical analysis, which helps researchers turn raw data into meaningful conclusions.
In this article, you’ll discover:
- The difference between descriptive and inferential statistics
- Practical medical examples for each
- When to use one or both methods
- Common mistakes to avoid
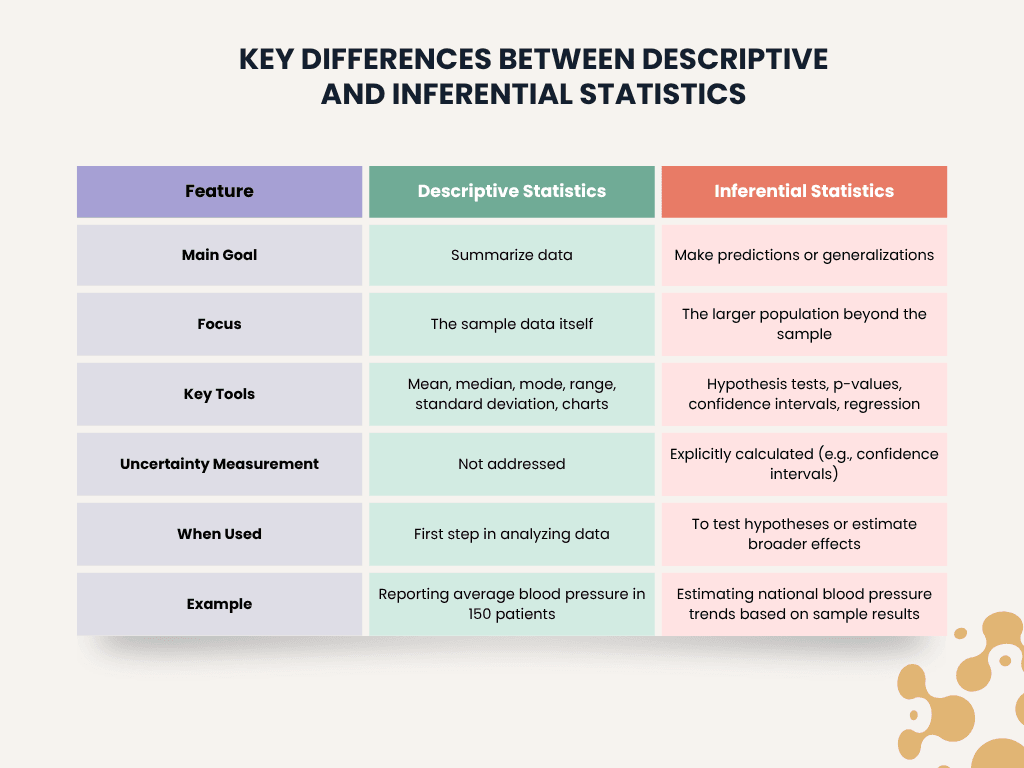
Key Differences Between Descriptive and Inferential Statistics
Both descriptive and inferential statistics serve distinct purposes in medical research. Understanding their differences helps ensure studies are properly designed, data is accurately interpreted, and conclusions are reliable.
| Feature | Descriptive Statistics | Inferential Statistics |
| Main Goal | Summarize data | Make predictions or generalizations |
| Focus | The sample data itself | The larger population beyond the sample |
| Key Tools | Mean, median, mode, range, standard deviation, charts | Hypothesis tests, p-values, confidence intervals, regression |
| Uncertainty Measurement | Not addressed | Explicitly calculated (e.g., confidence intervals) |
| When Used | First step in analyzing data | To test hypotheses or estimate broader effects |
| Example | Reporting average blood pressure in 150 patients | Estimating national blood pressure trends based on sample results |
In practice, researchers often begin with descriptive statistics to understand the basic features of the data before applying inferential methods to test hypotheses or estimate broader effects.
Descriptive Statistics Explained
Descriptive statistics help organize raw data into understandable summaries. Instead of reviewing hundreds of individual patient records, researchers can quickly see overall patterns in the data.
Definition and Purpose of Descriptive Statistics
Descriptive statistics are used to summarize the main features of a dataset. They provide a simple snapshot of the data without making generalizations beyond the sample. In medical research, this helps describe patient characteristics, treatment outcomes, or disease trends.
For example, a study measuring the blood pressure of 200 patients might report the average systolic blood pressure, the range of values, and how spread out the measurements are.
Measures of Central Tendency
Central tendency shows where most values in the dataset fall:
- Mean (Average): The sum of all values divided by the number of values.
Example: The average BMI of 200 patients. - Median: The middle value when data is ordered from lowest to highest.
Useful when data has outliers, such as very high cholesterol readings. - Mode: The most frequently occurring value in the dataset.
For instance, the most common number of medications taken by patients.
Measures of Dispersion
Dispersion describes how spread out the data points are:
- Range: The difference between the highest and lowest values.
- Variance: The average squared deviation from the mean.
- Standard Deviation: The square root of variance, showing how much values typically differ from the mean.

In clinical trials, a high standard deviation might suggest wide variability in patient responses.
For more details on measures of variability used in healthcare research, refer to This article discusses statistical measures of variability.
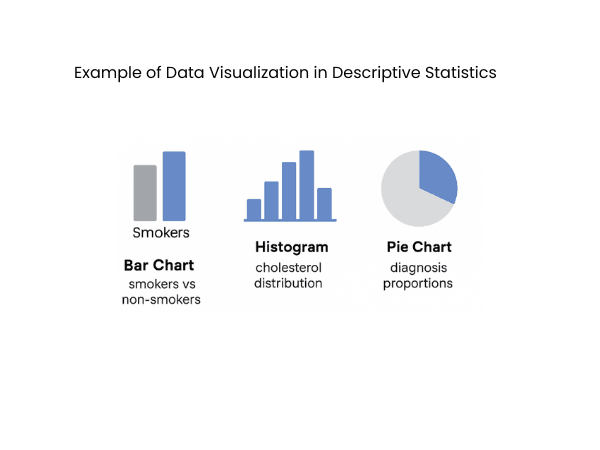
Data Visualization in Descriptive Statistics
Visual tools make descriptive statistics easier to interpret:
- Bar charts: Compare categories (e.g., number of smokers vs non-smokers).
- Histograms: Show the distribution of continuous variables (e.g., cholesterol levels).
- Box plots: Display the range, median, and outliers.
- Pie charts: Useful for showing proportions, such as distribution of patients by diagnosis category.
These types of graphical representations make it easier to communicate results to both clinical teams and non-technical audiences.
Inferential Statistics Explained
While descriptive statistics describe data from a specific group, inferential statistics allow researchers to extend conclusions beyond the study sample. In medicine, it’s often impossible to study every patient with a condition. Inferential methods use carefully selected samples to make predictions or test hypotheses about larger populations.
Definition and Purpose of Inferential Statistics
Inferential statistics estimate characteristics of a population based on sample data. They help determine whether observed results are likely to reflect true effects or are due to random chance.
For example, a new cancer treatment tested on 500 patients may show improved survival rates. Inferential statistics help estimate whether this effect would likely apply to all patients with the same condition.
Sampling Methods
Accurate inference depends on proper sampling. A sample must represent the target population to avoid biased results.
- Simple random sampling: Every individual has an equal chance of selection.
- Stratified sampling: The population is divided into groups (e.g., age or gender), and samples are drawn from each group to ensure representation.
- Convenience sampling: Easier but more prone to bias; often used in early-stage or exploratory studies.
For detailed guidance on sampling strategies in clinical research, see the NIH Sampling Methods in Clinical research.
Hypothesis Testing Basics
Hypothesis testing evaluates whether differences observed in the sample reflect real effects in the population.
- Null Hypothesis (H₀): Assumes no difference or effect.
- Alternative Hypothesis (H₁): Assumes there is a true difference or effect.
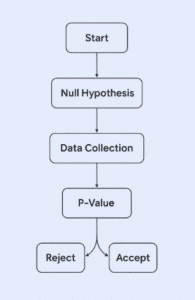
Statistical tests generate a p-value indicating how likely the observed results would occur if the null hypothesis were true.
For example, if a p-value is 0.03, there’s a 3% chance the results are due to random variation, suggesting a meaningful effect.
Confidence Intervals
A confidence interval gives a range of values likely to include the true population effect.
- A 95% confidence interval means that if the study were repeated many times, 95% of the intervals would contain the true value.
- Narrow confidence intervals suggest more precise estimates.
In a study of blood pressure medication, a 95% confidence interval might estimate that the true average reduction in systolic blood pressure falls between 8 and 12 mmHg.
For a deeper explanation of confidence intervals applied in clinical research, refer to this NLM Confidence Intervals Guide.
Regression and Correlation Analysis
Inferential methods also explore relationships between variables:
- Correlation measures how strongly two variables move together.
- Regression analysis models the relationship, allowing for prediction and adjustment for other factors.
Regression models estimate how one or more independent variables (such as age, medication dose, or lifestyle factors) affect a dependent variable, like blood pressure or cholesterol levels.
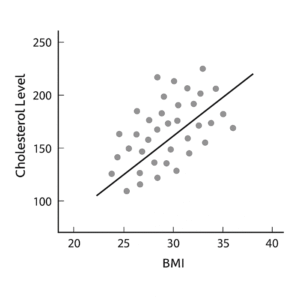
Regression methods are widely used to analyze relationships between clinical risk factors and outcomes. See this article Regression Analyses and Their Particularities in Observational Studies for further reading.
When to Use Descriptive vs Inferential Statistics
In most medical studies, both descriptive and inferential statistics are used — but at different stages and for different purposes.
Descriptive statistics are typically used at the start of any analysis to provide a clear overview of the data collected:
- Summarize patient characteristics (e.g., average age, gender distribution)
- Identify outliers or unusual patterns
- Check data quality before running more advanced analyses
Inferential statistics are applied when the goal is to answer research questions that go beyond the specific sample:
- Testing whether a new treatment is better than standard care
- Estimating disease prevalence in the wider population
- Predicting outcomes based on patient risk factors
Example:
A hospital conducts a study on a new diabetes drug:
- Descriptive statistics: The researchers report the average reduction in blood sugar levels among the 200 participants.
- Inferential statistics: They use hypothesis testing and confidence intervals to estimate how likely the drug would be effective for all patients with diabetes.
Whether analyzing a small clinic’s data or estimating trends across an entire population, using the right statistical approach is essential for producing reliable results.
Common Pitfalls to Avoid
Even with good data, mistakes in applying or interpreting statistics can lead to misleading conclusions. Here are common errors seen in medical research:
Misinterpreting Descriptive Statistics as Inferential
Reporting an average value from a sample does not automatically mean that result applies to the broader population. Without proper inferential testing, researchers risk overgeneralizing based on limited data.
Overgeneralizing from Small Samples
Small sample sizes often produce unstable results. Inferential methods rely on adequate sample sizes to minimize random error and improve precision.
Ignoring Variability
Focusing only on averages can hide important variations in patient responses. Always consider measures of dispersion to understand variability.
Overreliance on P-Values Alone
A statistically significant p-value does not always mean the result is clinically meaningful. Clinical importance should also consider effect size and confidence intervals.
Misinterpreting p-values is a frequent issue in published medical studies.
Conclusion
Both descriptive and inferential statistics are essential tools in medical research. Descriptive statistics provide a clear summary of data collected from a study, helping researchers understand patterns and variability within the sample. Inferential statistics allow those findings to be extended to larger populations, guiding clinical decisions, shaping public health policies, and advancing medical knowledge.
By understanding when and how to apply each method, healthcare professionals and researchers can interpret data more accurately and avoid common mistakes that lead to misleading conclusions.
FAQs
Descriptive statistics summarize data from a sample, showing patterns such as averages and variability. Inferential statistics use sample data to make generalizations about a larger population.
An example is reporting the average cholesterol level in a group of 300 patients.
An example is using data from a clinical trial to estimate how effective a new drug might be for all patients with a certain disease.
Descriptive statistics: summarize data already collected.
Inferential statistics: make generalizations about populations based on samples.
Predictive statistics: forecast future outcomes using existing data.
Yes. Most medical studies begin with descriptive statistics to summarize the sample, followed by inferential statistics to test hypotheses or estimate broader effects.
